온라인강의
강사명Yi-Hung Chen
강의시간24분
강의개설일2025-12-10
강의소개
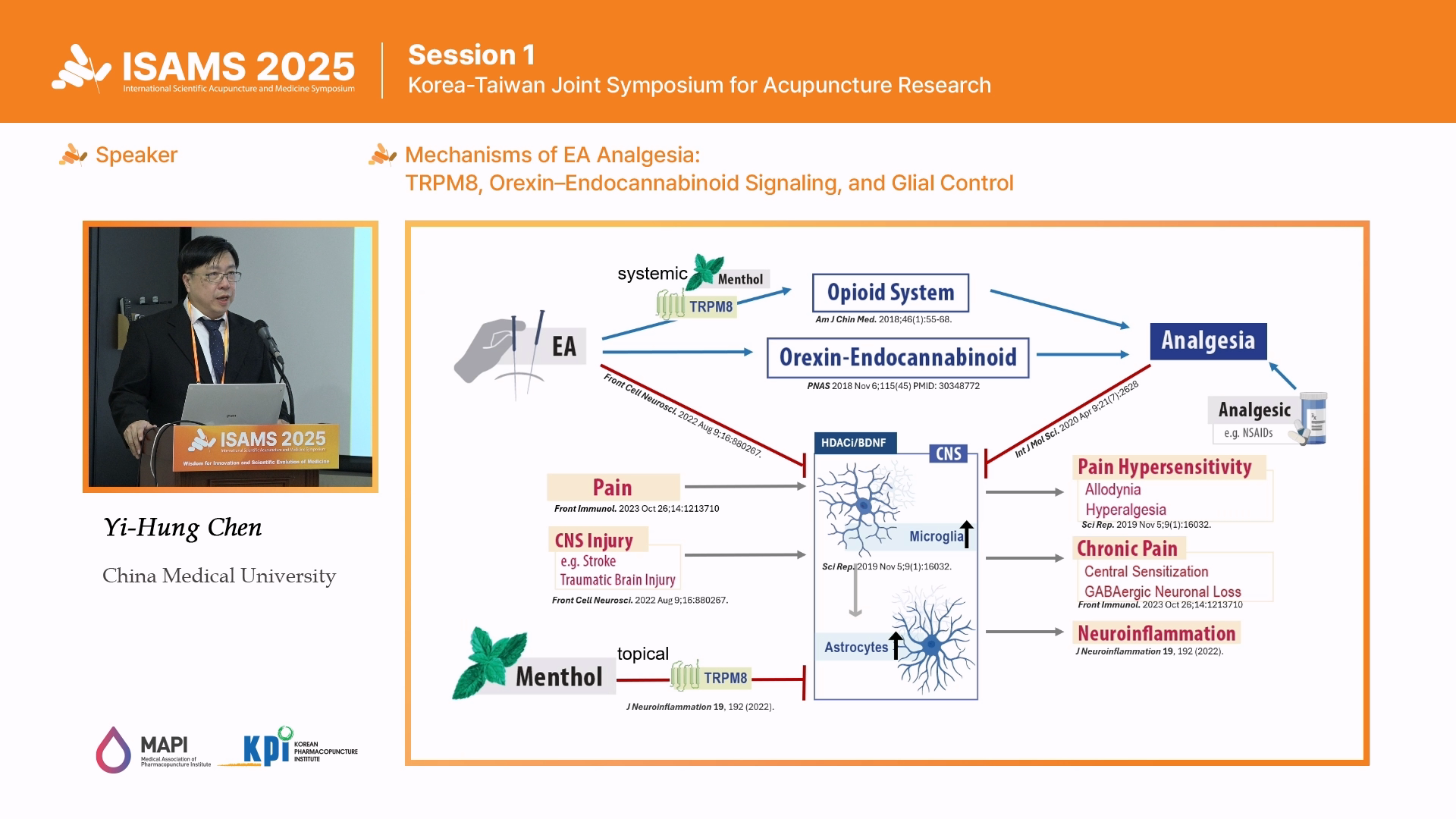
Acupuncture—the stimulation of defined body points with needles—has been practiced for ~2,500 years and is recognized by
the WHO for multiple indications. Electroacupuncture (EA), developed in the 1950s for surgical anesthesia, applies controlled
electrical currents through needles and produces reliable analgesia. This lecture interprets the accompanying figure to propose
an integrated CNS framework: EA activates peripheral afferents, reshapes spinal and supraspinal circuits, and engages both
opioid and non-opioid mechanisms. Early work established endogenous opioids; recent studies define a parallel orexin
endocannabinoid pathway that operates independently of opioids. Our new research identifies TRPM8 (transient receptor
potential melastatin 8)—the cold/menthol-gated ion channel—as a mechanistic gate for EA: intact TRPM8 permits recruitment
of endogenous opioids, whereas its inhibition or deletion shifts analgesia toward cannabinoid signaling. Converging on
neuroimmune targets, EA suppresses microglial and astrocytic activation, lowers pro-inflammatory mediators, and mitigates
central sensitization and GABAergic dysfunction—the drivers of allodynia, hyperalgesia, and pain chronification. These glial
centric effects also confer neuroprotection after CNS injury (e.g., stroke, traumatic brain injury).
Translationally, we show that: (i) EA at clinically relevant acupoints (e.g., PC6) alleviates pain via the orexin–endocannabinoid
axis and retains efficacy in opioid-tolerant states; (ii) EA reduces glial reactivity and neuroinflammation after experimental brain
trauma; and (iii) EA relieves severe dental pain and may limit the transition to chronic pain (e.g., irreversible pulpitis).
Together, these data position EA as a multimodal, non-pharmacologic strategy that coordinates opioid and non-opioid systems while
reprogramming neuroimmune responses—supporting evidence-based use of EA for pain management and neuroprotection.
강사소개
Professor Yi-Hung Chen is Associate Dean of the College of Chinese Medicine
at China Medical University and Director of the International Master’s Program in Integrative
Health. He received his Ph.D. in Pharmacology from National Taiwan University and has worked at Temple University
in the United States as a visiting scholar.
Professor Chen’s work integrates basic and clinical research to investigate pain relief and neuroprotection mechanisms
of acupuncture through modern biomedical approaches. His research has revealed non-opioid mechanisms of
electroacupuncture analgesia, such as activating the orexin and endocannabinoid systems via median nerve stimulation to
modulate pain in the midbrain, a study published in PNAS. He also explores neuroprotective strategies in animal models of
Parkinson’s disease and dental injury, focusing on factors like BDNF, HDAC, and microglial activation. Recently, his team
has studied the potential of topical menthol to activate TRPM8 channels through the skin, offering a possible neuroprotective
approach for ischemic stroke. Professor Chen’s work advances innovative strategies for stroke rehabilitation, chronic pain,
and neurodegenerative diseases, contributing to the modernization and global integration of traditional Chinese medicine.